PELVIC PROLAPSE
What is Pelvic Organ Prolapse
Pelvic organ prolapse occurs when muscles and ligaments in the pelvic floor are stretched or become too weak to hold the organs in the pelvis. This is not life-threatening, but can cause pain and discomfort and have a major impact on your day to day quality of life.
Potential causes that weaken and stretch the pelvis muscles include:

- Pregnancy and childbirth
- Aging and menopause
- Obesity
- Fibroids or pelvic tumors
- Long-term (chronic) coughing
- Long-term (chronic) constipation
- Lifting heavy objects
- Certain genetic conditions
- Prior pelvic surgery
- Some neurological conditions or spinal cord injury
How to know if you have pelvic prolapse?
The signs and symptoms of pelvic organ prolapse vary from woman to woman depending on the type of prolapse and how far it has advanced.
Mild prolapse may result in pressure or dragging sensation in your pelvic area, particularly if you have been standing for a long time.
As the prolapse becomes more severe, you may notice increasing discomfort and one or more additional symptoms including:
- Problems controlling your bladder
- Difficulty emptying your bladder
- Leaking urine during everyday activities that put pressure on your abdomen (stress urinary incontinence)
- Constipation or other bowel problems
- Discomfort or pain in your lower pelvis
- Back pain
- A feeling that something is stuck or falling out of your vagina
- Discomfort or pain during intercourse
- A lump in your vagina
- Unusual bleeding or discharge
Types of Prolapse
Your doctor will assess which type of prolapsed that affects you. It is possible that you may have more than one type at the same time.
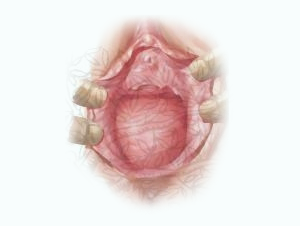
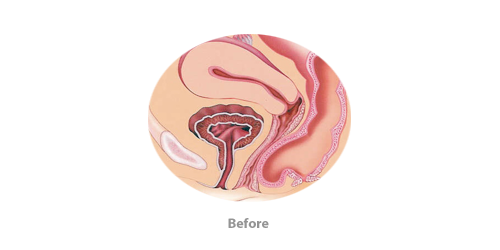
Cystocele
As a result of childbearing, there can be spreading and tearing of some of the principal muscular supports of the vagina which can lead to the bladder pushing forward and downward to form a hernia sac known as a cystocele. The size of this defect has to do with the number of previous deliveries as well as the size of the baby and other factors prior to delivery. A cystocele does not necessarily cause symptoms; however, if it is large enough, it may produce symptoms of urinary retention, stasis of urine leading to recurrent infections, burning on urination, increased frequency, nocturia and stress urinary incontinence.


![Description: C:\Documents and Settings\Administrator\Local Settings\Temporary Internet Files\Content.Word\rectocele-and-cystocele-pictures-i2[1].jpg](images/pelvic_prolapse_clip_image006.png)
Rectocele
As with cystocele, childbearing produces tearing higher in the posterior vagina extending laterally to allow herniation of the delicate tissue surrounding the rectum. This can cause various degrees of prolapse of the pelvic floor called a rectocele. The rectocele is usually graded by their size of the hernia sac to or beyond the opening of the vagina. Rectoceles often occur in conjunction with additional prolapse such as cystocele and may be completely asymptomatic. Patients may also complain of a dull aching sensation. More commonly, they may complain of difficulty evacuating the rectum when it is full of stool. This may require a vaginal finger to help evacuate a hardened stool.

Other types of prolapsed include
Uterus prolapse – a uterine prolapse occurs when the uterus drops down into the vagina.

Small bowel prolapse – an enterocele occurs when the small intestine drops down between the back of the vagina and the rectum. This may occur at the same time as prolapse of the uterus or rectum.
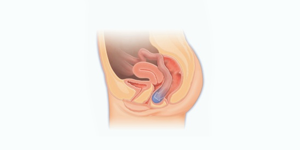
Vaginal vault prolapse – a vaginal vault prolapse can be found when the top of the vagina falls in on itself. This can only occur if a woman has had a hysterectomy (an operation to remove the uterus).

Treatment
There are different treatment options available and your doctor will be able to help you find the best solution for you. This will depend on the type and cause of your prolapse as well as your plans for the future, such as whether you are planning to become pregnant. It is common for treatment to start with a non-surgical approach such as Kegel exercises, a pessary (a device worn in the vagina for support), estrogen supplementation, electrical stimulation, or biofeedback. However, many cases of pelvic organ prolapse may only be corrected with surgery.
Surgical Treatment
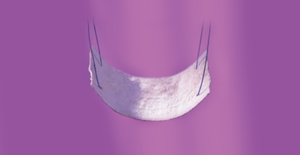
A surgical treatment option for pelvic organ prolapse involves fitting a special graft to repair the pelvic floor. The graft can support the affected organ(s) and relieve your symptoms.In this office, the procedure is done by utilizing a unique biologic graft material which does not have the inherent complications of a vaginal mesh graft.
The procedure is completed as a combined team approach with both a Gynecologist and Urologist assisting each other.
The biologic graft used is called Axis™. Axis is composed of natural, safe and reliable bioimplant material created from donated human tissue, which is placed through a rigorous Tutoplast cleaning process to remove any and all transmissible pathogens. Tutoplast processed tissues have been successfully implanted on over 2 million patients without a single documented case of disease transmission. Axis has been implanted for over 10 years with over an 80% success rate for pelvic floor repair procedures. Once placed, the graft incorporates within your body’s own tissues to correct the prolapse by strengthening the pelvic floor muscles and keeping the organs in place.
- Mesh Grafts
- Polypropylene material used for bridging tissue and supporting organs.
- Biologic Grafts
- Tissue from patient, human donor or animal
-
Patient own grafts and cadaveric biologics are not part of the July 13, 2011 FDA safety communication
- Natural
- Processed from human donors
- Axis® Dermis tissue comes from the lower back
- Safe
- Been implanted for over 30 year with no disease transmission
- Goes thru a rigorous process called Tutoplast that gets rid of all forms of bacteria, DNA, RNA and any type of viruses.
- A completely sterile material
- Strong
- Due to the processing of the graft it remains very strong and allows for tissue growth
- 12 year data proves a >80% success rate
DERMIS GRAFT
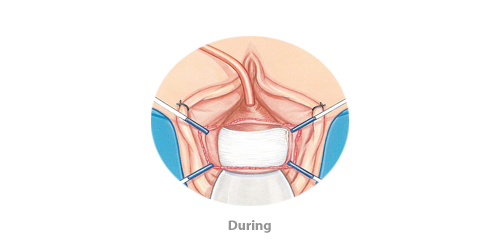
CYSTOCELE REPAIR
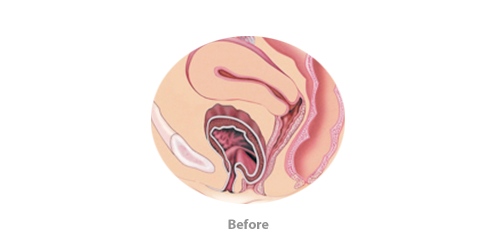

RECTOCELE REPAIR
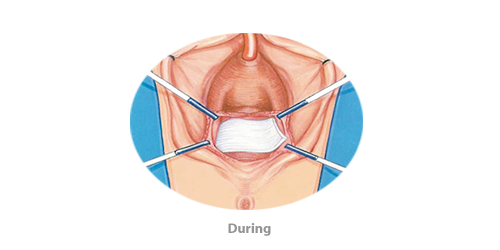

During Surgery
Surgery for pelvic organ prolapse is performed at a hospital under general anesthesia. The graft is inserted through a incisions in the vagina. After the prolapsed organs are restored to their natural position, the graft is placed above or below to reinforce the repair.After Surgery
After the surgery, you will generally be required to stay in the hospital overnight. It is normal to feel some discomfort and tiredness for one or two days after the procedure. During your recovery, it is important not to lift anything heavy or have sexual intercourse so that your body can heal and the new graft material can bind with your own tissues.Risks
Prolapse repair with a biologic material may not be suitable for every patient, and a thorough discussion between you and your doctor will enable both of you to determine if this technique is right for you.Education
Many women find it difficult to speak about pelvic organ prolapse. Fortunately, it will become easier to discuss with time, especially now that you have educated yourself about these conditions. Remember that it is a common problem and your doctor has seen many other patients with pelvic organ prolapse before.