Incontinence
Urinary incontinence is the involuntary loss of urine from the body. It affects over 13 million Americans, 85% of whom are women. Urinary incontinence that occurs with straining or with activities is known as stress urinary incontinence (SUI).
There have been many advances in the treatment of urinary incontinence. “No woman should feel that poor urinary control is not correctable and simply a fact of aging.”

Typical activities that can provoke leakage of urine are running, jumping, coughing, sneezing, laughing, and even sexual intercourse. While incontinence is often considered an aspect of aging, in many cases it can be treated. Multiple treatment options exist for patients. If medications, fluid restriction and pelvic floor muscle exercises do not improve a woman’s urinary incontinence, then a pessary may be utilized in the vagina to provide relief. When none of the above non-surgical options reduce symptoms, surgical correction may be considered.
Quiz
- Do you lose urine when you sneeze or cough?
- Do you jump, run, swing a golf club or tennis racquet and lose urine?
- Do you laugh at a party and have to excuse yourself because you have wet your clothing?
- Do you arrive at a restaurant and your first stop is the bathroom prior to dinner?
- Do you go to the mall and need to map out restrooms before you can shop?
- Do you need to urinate prior to being intimate to prevent embarrassing urine loss?
- Did you know that 50% of women may require incontinence surgery if they have had at least one vaginal childbirth and are now over the age of 40?
If you answered yes, to any of these questions you may have a type of incontinence.
Incontinence may manifest itself as constant dribbling or as intermittent voiding without the individual being aware of the need to void. Some patients have had extreme urgency with little or no warning and are unable to make it to the bathroom. Incontinence may occur with some maneuvers that increase intra-abdominal pressure. The clinical pattern of incontinence is useful. However, causes of incontinence often overlap.
- Urge incontinence is the uncontrolled urine leakage that occurs immediately after the irrepressible need to void. Urge incontinence is a common type of urine loss and is exacerbated by the inability to quickly reach the bathroom. In older women, atrophic vaginitis contributes to thinning irritation of the urethra and urgency.
- Stress incontinence is urine leakage due to an increase in intra-abdominal pressure such as coughing, sneezing, laughing, bending, lifting and exercising. This is a common type of incontinence largely because of childbearing and thinning of the vaginal wall. Stress incontinence may be more severe in obese women because of undue pressure on the bladder from the abdominal contents.
- Overflow incontinence is the constant dribbling of urine from an overly full bladder. The volume tends to be minimal however leakage may be constant.
- Functional incontinence is urine loss that is due to cognitive or physical impairments. This may be due to the neural pathways being interrupted such as with CVA (stroke), spinal cord injury or dementia which does not allow the maintenance of normal urine continence.
What to expect at the doctor’s office
It is important to diagnose your incontinence correctly to ensure the appropriate treatment option is selected. Your physician will want a complete medical and surgical history, a list of all medication and supplements, as well as information about your urinary habits and all fluids consumed. It’s important to accurately describe the problems you are having, such as when and under what conditions leakage occurs.
It may be beneficial to track your voiding habits in a journal to share with your physician. A voiding diary should include information such as what you drink, number of times you urinate and if you have episodes of leakage.
Clinical Evaluation
All patients will have a comprehensive history and physical examination, which emphasizes the woman's urogenital tract. A focused physical examination assesses vaginal tissue and neighboring organ support. The tests are simple and relatively painless. Additional tests may be recommended or more sophisticated urodynamics may be completed to provide for accurate diagnosis and treatment for particular types of incontinence. Advanced Urodynamic testing is usually performed if the patient is not responding to conservative therapy and/or is considering surgery. See Urodynamic page under procedure menu.
Treatment Options
If you have been diagnosed with stress urinary incontinence, it is important to understand your options. Surgery is not suitable for everyone, and you should discuss all solutions available with your doctor.
Non-surgical options are pelvic muscle exercises, protective under garments, behavioral therapies, catheters, vaginal pessaries and bulking injections.
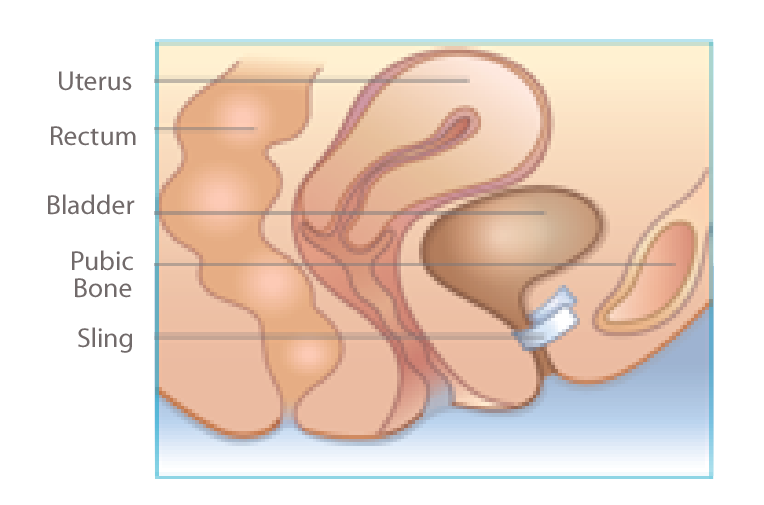
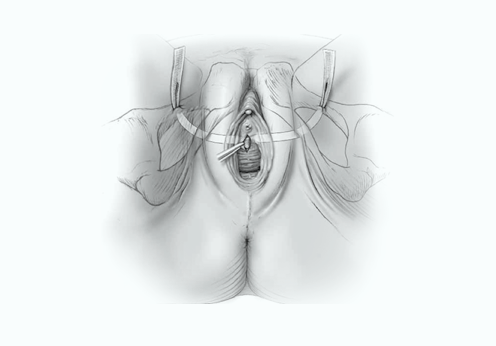
Surgical options are open bladder neck suspensions, and sling procedures. A sling procedure corrects stress incontinence by placing a small strip of synthetic material beneath the urethra, and like a backboard, it supports the urethra during straining maneuvers or other activities, and can prevent leakage from occurring.
What Happens During Surgery
A sling procedure is the most common minimally invasive surgical option to correct stress urinary incontinence. It is usually performed as an out-patient procedure in less than 30 minutes; however an overnight stay may be necessary especially if additional prolapse procedures are done concomitantly.
There are a variety of ways to place a sling, since there are many different types of slings available. The type of sling chosen is based on a number of factors, including the severity of incontinence, prior pelvic surgery, patient and physician preference.
What happens after the surgery?
Your doctor will discuss post-operative instructions and recovery time with you. In general, expect a period of time to refrain from exercise, physical activity, straining and sexual activity. It is important to know that following a sling procedure, future pregnancies may negate the effects of the surgical procedure, and you may once again become incontinent.
Although every patient’s recovery is different, there are general recovery guidelines that apply to most sling procedures. A sling procedure is a minimally invasive surgery; however, an overnight hospital stay may be required. You may experience some minor discomfort and fatigue during the first 24 to 72 hours after surgery.
Your doctor will provide specific details about your individual recovery process, and he or she may have other recommendations based on your individual needs. Please follow your physician’s directions closely.
Returning to an active lifestyle
Many women find it difficult to talk about incontinence due to potential embarrassment about the subject or the intimate nature of the problem. There are many options for treating or managing incontinence and it is important to discuss all of the options with your doctor.
By treating your incontinence successfully, you are getting back in control and are free to return to the active lifestyle you have always enjoyed.